Pipeline
THERAPEUTIC PIPELINE
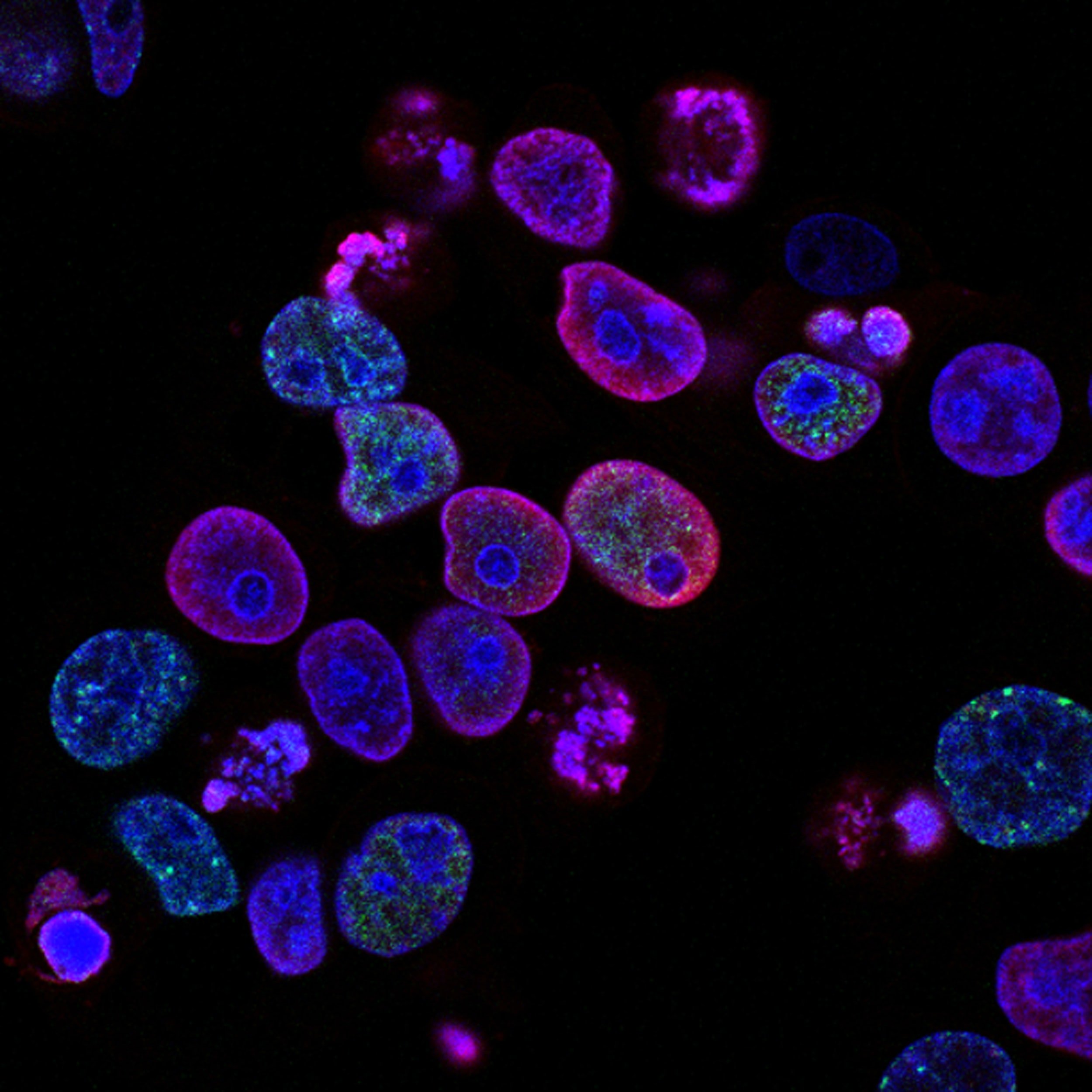
ISCO scientists are using human parthenogenetic stem cells (hpSC) to treat severe diseases of the central nervous system, joints and liver, where cell therapy has shown clinical benefit but treatment options are limited by the availability of human cells.
The hpSC are a promising therapeutic source because of their wide variety of treatment applications and ease of expansion. They also offer an abundant renewable resource, in contrast to scarce organ transplants and fetal tissue.
-
ISC-HPNSC®
We have derived a homogenous population of neural stem cells (ISC-hpNSC®) from hpSC through a chemically directed differentiation protocol (1). The ISC-hpNSC® were expanded and cryopreserved into master and working cell banks under cGMP. The cells underwent strict quality control measures testing each cell bank for cell identity, potency, purity and sterility to ensure the safety of the final product. Our clinical grade ISC-hpNSC® express the appropriate neural stem cell markers, have a normal karyotype and are clear of microbial and viral contaminants.
Parkinson’s Disease
According to the Parkinson’s Disease Foundation, an estimated seven to 10 million people worldwide live with Parkinson’s disease. As many as one million patients live in the United States, more than the combined total of people diagnosed with multiple sclerosis, muscular dystrophy, and Lou Gehrig’s disease. The total direct and indirect cost of Parkinson’s disease is estimated to be nearly $25 billion per year in the United States.At ISCO, unlike conventional treatments for Parkinson’s disease that do not stop disease progression, the company’s ISC-hpNSC® offers to be a disease modifying treatment that could potentially slow down disease progression. The ability of our stem cells, ISC-hpNSC® to differentiate into dopaminergic neurons as well as express brain-protecting neurotrophic factors offers a new approach to treating Parkinson’s disease. We believe that a one-time transplant of ISC-hpNSC®, into the brain of Parkinson’s patients, replacing the dead and dying dopaminergic neurons and offering protection and neurotrophic support to the remaining neurons, could alleviate symptoms of the disease and prevent further deterioration.
Transplantation of ISC-hpNSC® was shown to be safe, well tolerated and effective in treating preclinical models of PD (2,3). ISC-hpNSC® promoted behavioral recovery without dyskinesias and increased striatal dopamine (DA) concentration, fiber innervation and number of DA neurons in comparison to control animals. Based on these extensive preclinical studies, the Australian Therapeutic Goods Administration and Human Research Ethics Committee have granted approval to conduct a dose escalating Phase I study.
Traumatic Brain Injury
According to the CDC, roughly 30% of all injury related deaths are caused by Traumatic Brain Injury (TBI). For survivors, lasting effects from the injury including cognitive function, memory loss, depression, and altered vision, can remain. Roughly 2.5 million emergency room visits, hospitalizations, and deaths occurred in 2010, with TBI contributing to 50,000 deaths.In addition, TBI can cause epilepsy and patients are at risk of Alzheimer’s and Parkinson’s diseases and other brain disorders that become prevalent with age. In the acute phase of TBI, significant breakdown of the blood brain barrier is quite common with subsequent inflammation. ISC-hpNSC® provides neurotrophic support and neuroprotection by the release of neurotrophic cytokines which may dampen an inflammatory reaction and help restore the blood brain barrier. For the more chronic phase of TBI, ISC-hpNSC is capable of repairing damage from Parkinson’s disease and stroke. It is therefore possible that ISC-hpNSC® may alleviate the non-specific damage inflicted by TBI.
Ischemic Stroke
The National Stroke Association lists stroke as a leading cause of death in the United States, and a leading cause of serious, long-term adult disability. Approximately 795,000 strokes occur each year, taking a life approximately every four minutes. About 87% of strokes are ischemic. The estimated direct and indirect cost of stroke in the United States in 2010 is $73.7 billion.Despite its prevalence, there are no medical therapies for alleviating the chronic functional impairments following stroke. Human fetal neural stem cell transplants have been shown to produce some recovery in animal models of stroke, but ethical consideration and a short supply of fetal tissue limits this approach. Our clinical grade ISC-hpNSC® have been demonstrated to be safe, and provide significant functional improvement in a stroke mouse model. ISC-hpNSC® have the ability to become a variety of neural cell types replacing the brain cells lost after a stroke. ISC-hpNSC® also provide neurotrophic support and neuroprotection by the release of neurotrophic cytokines. Additionally, ISC-hpNSC have immunomodulatory properties that reduce the inflammatory response caused after the stroke. The multiple mechanisms of action make ISC-hpNSC® an ideal therapeutic candidate for stroke.
CHONDROSTEM
Osteoarthritis (OA) is a degenerative joint disease characterized by progressive erosion of the articular cartilage which leads to joint pain, stiffness, and impaired mobility. OA affects over 27 million Americans and the combination of arthritis and other rheumatic conditions have estimated medical costs of as much as $128 billion (Centers for Disease and Prevention 2007). Current cell therapy and tissue engineering therapeutic strategies for OA utilize expanded chondrocytes or autologous mesenchymal stem cells (MSCs). The differentiation protocols generate fibrocartilaginous tissues for transplantation which are mechanically defective.
Our ChondroStem technology results in regenerating cartilage with enhanced cell viability by increasing the components involved in rebuilding cartilage: glycosaminoglycans, collagen type II, aggrecan and sulfated proteoglycans. We are utilizing 3D bio-printing capabilities to generate cartilage suitable for repair of damaged or osteoarthritic joints. We believe that ChrondroStem will be a superior therapeutic candidate for osteoarthritis and other rheumatic conditions.
CYTOHEP
We have derived a homogenous population of hepatocyte-like cells (CytoHep) from hpSC. CytoHep was manufactured under cGMP with a novel method to derive high-purity definitive endoderm. Based on reproducing features of the normal human embryonic microenvironment, the highly enriched population of hepatocyte-like cells that are characterized by expression of hepatic lineage markers, indocyanine green clearance, glycogen storage, and cytochrome P450 activity (4,5). CytoHep can be used for the treatment of several liver diseases.
Metabolic Liver Diseases
Crigler-Najjar syndrome is a serious inherited metabolic liver disease where the liver lacks a critical enzyme responsible for processing the metabolic toxin bilirubin. The absence of this enzyme causes a build-up of bilirubin in the blood which can lead to brain and nerve damage. The most severe form of the syndrome results in early death; however, transplanting liver cells into a patient’s liver can help alleviate the symptoms of the disease.
Our CytoHep behave similarly to primary hepatocytes. Implanting CytoHep in a pre-clinical animal model of Crigler-Najjar syndrome has shown positive benefits. CytoHep transplant lead to liver engraftment and a significant reduction of serum bilirubin levels compared with controls (6).
Liver Cirrhosis
Liver Cirrhosis is the scarring of the liver due to chronic hepatitis infection, alcoholism, autoimmune diseases, genetic diseases or enzymatic deficiencies. According to the National Institute on Alcohol and Alcoholism, cirrhosis is the 12th leading cause of death in the U.S. as of 2007, with 48% alcohol related. Roughly 17,000 people are awaiting liver transplants, with roughly 20% dying each year before a suitable donor can be found.
CytoHep offers the possibility to generate a functional tissue utilizing our 3D bio-printing capabilities. In vitro, CytoHep expresses hepatic lineage markers and exhibits indocyanine green clearance, glycogen storage, and cytochrome P450 activity, and showed sustainable engraftment in a pre-clinical animal model, making it a leading candidate for tissue generation (4,5).
References
1. Deriving dopaminergic neurons for clinical use. A practical approach. Gonzalez R, Garitaonandia I, Abramihina T, Wambua GK, Ostrowska A, Brock M, Noskov A, Boscolo FS, Craw JS, Laurent LC and others. Scientific Reports 2013;3(1463):1-5.
2. Proof of concept studies exploring the safety and functional activity of human parthenogenetic-derived neural stem cells for the treatment of Parkinson’s disease. R. Gonzalez, I. Garitaonandia, A. Crain, M. Poustovoitov, T. Abramihina, A. Noskov, C. Jiang, R. Morey, L.C. Laurent, J.D. Elsworth, E.Y. Snyder, D.E. Redmond Jr, and R. Semechkin. Cell Transplantation 2015;24(4):681-90.
3. Neural stem cells derived from human parthenogenetic stem cells engraft and promote recovery in a nonhuman primate model of Parkinson’s disease. R. Gonzalez, I. Garitaonandia, M. Poustovoitov, T. Abramihina, C. McEntire, B. Culp, J. Attwood, A. Noskov, T. Christiansen-Weber, M. Khater, S. Mora-Castilla, C. To, A. Crain, G. Sherman, A. Semechkin, L.C. Laurent, J.D. Elsworth, J. Sladek, E.Y. Snyder, D.E. Redmond Jr., R.A. Kern. Cell Transplantation 2016. PMID: 27213850. DOI: 10.3727/096368916X691682
4. Derivation of high-purity definitive endoderm from human parthenogenetic stem cells using an in vitro analog of the primitive streak. N. Turovets, J. Fair, R. West, A. Ostrowska, R. Semechkin, J. Janus, L. Cui, V. Agapov, I. Turovets, A. Semechkin, M. Csete and L. Agapova. Cell Transplantation 2012;21(1):217-234
5. Human parthenogenetic stem cells produce enriched populations of definitive endoderm cells after trichostatin A pretreatment. N. Turovets, K.A. D’Amour, V. Agapov, I. Turovets, O. Kochetkova, J. Janus, A. Semechkin, M.A. Moorman, L. Agapova. Differentiation. 2011 Jun;81(5):292-298.
6. Agapova L, Ostrowska A, Christiansen-Weber T, Chu T, Semechkin R. Human parthenogenetic stem cell-derived hepatocytes correct serum bilirubin in Gunn rats. 11th Annual Meeting of International Society for Stem Cell Research. Boston, MA USA 2013.n goes here